UK hospitals have been relatively empty compared to Europe – so why is the NHS struggling?

As politicians and clinicians alike proclaim we are in the hardest haul of the pandemic, and tearful tales from intensive care wards are the stuff of every news broadcast, is the NHS on the brink of collapse? Is the risk of running out of intensive care beds, as Boris Johnson warned this week, “very substantial”?
Clearly, the pressure caused by the new strain, B-117, is great. Across the country, Tier 4 restrictions, which kept the old version of the virus under control, saw a tenfold increase in variant cases every three weeks.
That explains the abrupt halt in the decline of UK cases after October and November’s second peak. In other comparable countries such as France and Italy, 2020 shows two clear, smooth arcs of hospital admissions – spring and autumn, up and down.
Not here. Here the autumn downturn was rudely interrupted then radically reversed. On December 2, three weeks after the November 11 peak of 1,711, daily admissions were down to 1,262. But the next day they started climbing again, up to 1,337. A month later there were 3,351 daily Covid-19 admissions.
Even so, on that day, January 3, NHS England reported that of its 90,872 general beds, only 79,301 were occupied, with patients suffering all manner of ailments, including Covid-19, leaving 11,571 – or 12.7 per cent – of beds available.
Perversely, that empty rate was greater than the pre-pandemic norm, which stood at 9.3 per cent, according to the King’s Fund think tank.
Indeed, total patient numbers are still recovering from last summer, when occupancy plummeted, with beds emptied to await the expected Covid-19 influx and patients staying away from hospital.
Data shows that an average of 90,309 beds were occupied in the first three months of last year, but that number from March to June fell to an unprecedented 58,005.
Such comparisons are not perfect. Hiving off sections of hospitals to prevent Covid-19 infections spreading meant a loss of almost 10,000 beds. “Hospitals will experience capacity pressures at lower overall occupancy rates than would previously have been the case,” the NHS warned.
By the end of January 3, the total in hospitals suffering from the virus was 26,626, of whom 24,316 were in general beds – exactly 30 per cent of all patients in the NHS.
The other 2,310 Covid-19 patients were ill enough to be on mechanical ventilation, meaning they were in critical care units – taking 58 per cent of the 3,981 critical care beds occupied that day.
Again, even then another 970 critical beds – 19.5 per cent – remained unoccupied, according to the NHS’s own data, almost precisely the usual unoccupied rate, which King’s Fund analysis puts at 19.7 per cent.
The fact that such a margin continued to exist in exceptional times was thanks to the work done since the start of last year to expand the number of critical care beds – from 4,123 a year ago to 4,951 on January 3 this year. A decade ago there were 3,550.
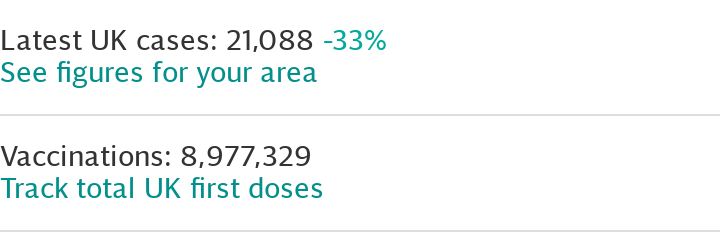
Things continued to get worse for the next three days. On January 6, Covid-19 admissions hit a record 3,967. After that, however, they began to decline again – if very slowly. Matt Hancock, the Health Secretary, said on Wednesday that he hoped the peak had been reached. By January 10 admissions were at 3,571 and the rolling average was down, too.
Naturally, there will be a lag before that drop in admissions equates to relief for the NHS. But if January 6 does turn out to have been a peak, then the NHS will have coped. On that day it had 4,297 critical care patients, leaving 871 (or 16.8 per cent) free beds as, heroically, more and more were made available throughout the week.
On January 4, critical care capacity was 4,976. A week later it was 5,503. In general wards, the situation was less intense. There, 82,887 of 92,555 beds were occupied, leaving 10.44 per cent free.
The problem was local pinch points. At Homerton University Hospital NHS Foundation Trust in London, for example, all critical care beds were occupied. King’s College Hospital was also at breaking point with 112 of 114 beds taken. The stress it faced was clear as, on January 7, 53 new critical care beds were made available, more than half of which were filled immediately.
But nationally, the NHS has not yet approached 100 per cent capacity.
There is, of course, room for further expansion in the seven temporary Nightingale hospitals. Last year ExCeL London offered 2,900 extra critical care beds, with another 500 in its equivalent in Yorkshire. Both went mostly unused. The ExCeL Nightingale has been reopened to take non-Covid patients from crowded London hospitals.
But if used as originally intended, and when beds in private facilities are co-opted, England edges towards 10,000 critical care places at the absolute limit.
On ventilators, too, there is also capacity. According to the National Audit Office, as the pandemic began last February/March, NHS England had 7,400 ventilators. By August, that total had hit 30,000 – some 10 times the current requirement.
The pressure point is instead on staff. Beds and ventilators require specialist doctors and nurses to operate. Rules have been relaxed to allow them to care for several critical patients at a time, rather than standard one-to-one treatment, and for non-specialist staff to help critical care nurses.
Now attention may well turn to the 35 countries beyond these shores with B-117. European nations have worried about the “UK strain” for weeks, fearing that their own second peaks may morph, as ours did, into much worse third peaks.
Already the decline in hospital admissions in Italy and France, which continued throughout December even as ours soared, has stalled. On that same January 3, cases in both countries ticked up again, after six weeks of steady falls.
The question is, will the novel strain be responsible for a cataclysm there? Because in each of 2020’s two waves – March/April and October/November – France and Italy had between two to three times as many patients per capita in hospital and in critical care as the UK.
At Italy’s absolute peak, 635 out of every million Italians were in hospital with Covid-19, with 67 per million in critical care. In France those figures were 513 and 107. By contrast, in the UK, they were 319 and 48.
Indeed, only now have our hospital admission and critical care rates surpassed those of France and Italy, after a terrible six weeks.
Such massive disparity between British and Italian and French hospital admission and critical care admissions in 2020 raises a potentially alarming question: why did so many more of them, per capita, end up in hospital than us? Were they more vulnerable?
The data suggests not. Italy’s population is a little older, but like that of France, much less obese than in the UK.
Did they simply make use of greater capacity? Because both countries were able to call on greater resources than the UK. In normal times France has more than twice the number of hospital beds per capita as the UK, and Italy almost twice as many critical care beds.
This, too, seems unlikely. Despite our comparatively smaller capacity, we did not reach it. Indeed, in general beds, UK hospitals were comparatively empty in 2020. Nightingales went unused.
This leaves a third possibility – the stiff upper lip.
Fearing that the NHS would be overwhelmed, did many sick people (not just those with Covid-19) who should have gone to hospital choose to stay away? One way of testing this is to look at the numbers of people dying at home instead of in hospital. According to the ONS, at April’s peak last year, some 4,834 people died at home – exactly double the usual figure of 2,400.
Compare that with France, where the number of people dying at home in March and April 2020 rose by just 32 per cent compared with 2019.
So was our stiff upper lip to blame for our excess mortality, the worst in Europe bar Spain?
If so, it is a reminder that grim warnings about NHS capacity, from the Prime Minister down, are a double-edged sword. Such warnings may be an effort to convince lockdown rule breakers to change their ways. But they may have the effect of persuading some among the far greater numbers of rule observers to stay away from the NHS when, in fact, they desperately need medical attention.
The situation is still very fraught in the UK. But declining admissions suggest there may now be a reason for cheer. By contrast, the worst may be to come on the Continent and beyond.
Last year stretched both France and Italy’s health services to the limit. Italy came within a few per cent of its usual general bed capacity, France the same with critical care.
A new peak on the scale that this country has just faced would put both France and Italy well beyond those normal limits. No wonder they are so desperate to avoid the super-transmissible strain now known as “le mutant britannique”.

 Yahoo Movies
Yahoo Movies 
